Key Points
- While the vitamin D3 molecule created in response to sunlight is the same as the molecule found in food and supplements, there are certain differences in how the body processes, absorbs, and utilizes the vitamin D
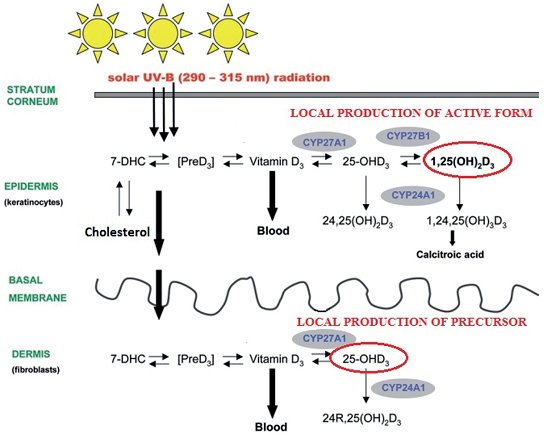
- Exposure of the skin to UVB radiation initiates the conversion of cholesterol to pre-vitamin D3, which can then be further converted into other photoproducts that have their own unique biological properties, possibly playing a role in reducing the risk of skin cancer; pre-vitamin D3 is also converted into other forms of vitamin D, including its active form, directly within the skin cells for their own use
- While vitamin D toxicity is possible to achieve from supplements, it is not possible when generating vitamin D from sun exposure; vitamin D3 generated by sunshine exposure is also available to the body 2-3 times longer than that taken orally
Vitamin D3 production is initiated in the skin upon exposure to ultraviolet B (UVB) radiation from sunshine and indoor lighting options containing UVB. Vitamin D can also be found in some foods and supplements, as vitamin D3 and D2. While the vitamin D3 molecule created in response to sunlight is the same as the molecule found in food and supplements, there are certain differences in how the body processes, absorbs, and utilizes the vitamin D. Watch the video snippets and read more below for several examples of these differences.
NOTE: When discussing vitamin D in this post, we are referring to vitamin D3 that is either being produced in the skin or taken orally, not vitamin D2. Vitamin D2 is only found in supplements and foods, and is not produced in response to sunlight.
What Happens with Vitamin D When it is Taken Orally?
Vitamin D3 found in supplements is ingested and absorbed through the gut. The amount absorbed in the gut depends on several factors, including digestive health, if taken with a meal, current medications, and others. Digestive conditions including irritable bowel disease, Crohn’s disease, and celiac disease can limit the absorption of vitamin D, and diseases of the liver (e.g. fatty liver), pancreas, gallbladder removal, or bariatric surgery bypassing the small intestine can all lead to trouble absorbing vitamin D.
The dose of vitamin D3 that is absorbed through the gut makes its way into the blood stream very quickly and all at once, and due to its short half-life, it is only available within the bloodstream for about 24 hours.
While a percentage of the vitamin D absorbed from the gut becomes bound to vitamin D binding protein (VDP) and albumin for transport in the bloodstream, that which is not converted and remains unbound is excreted through the liver and bile and into the feces.
What Happens with Vitamin D When it is Produced in the Skin?
Exposure of the skin to UVB radiation initiates the conversion of cholesterol to pre-vitamin D3, which can then be further converted into other photoproducts that have their own unique biological properties, possibly playing a role in reducing the risk of skin cancer. Pre-vitamin D3 is also converted into other forms of vitamin D, including its active form, directly within the skin cells for their own use, as illustrated in the diagram below.
When pre-vitamin D3 is made in the skin it is converted slowly into vitamin D and released into the bloodstream over a couple of hours, allowing the vitamin D to be available in the bloodstream 2-3 times longer than that absorbed through the gut.
Vitamin D Produced in the Skin Helps Protect the Skin
Studies have shown that vitamin D made in the skin has antioxidant effects that can decrease DNA damage in the skin cells and facilitate DNA repair directly upon any UV damage, help prevent cell death, and help protect from melanoma, a serious form of skin cancer. Furthermore, sensible exposure to sunlight actually protects the skin and deeper tissues from UV damage by increasing pigmentation (short term tanning and avoidance of sunburn) and thickening the outermost layer of skin – a process beneficial even for those with already darker skin.
In fact, keratinocytes, which make up over 90% of the outermost layer of skin, cannot rely on vitamin D3 from supplements. Keratinocytes must synthesize their own supply of vitamin D directly from sun exposure (as illustrated in the diagram above), or by topical application as described in a review by Bolerazska et al..
It is Not Possible to Become Toxic from Vitamin D Produced by Sun Exposure
Vitamin D toxicity is rare and usually caused by excessive vitamin D supplementation, which can lead to hypercalcemia (increased calcium in the blood), hyperphosphatemia (increased phosphate in the blood), and suppressed serum PTH concentrations. Symptoms include vomiting, nausea, abdominal pain, fatigue, and weakness. Most cases of vitamin D toxicity have been related to supplement manufacturing and labeling errors, as well as overdosing (seen in some cases with intakes of 50,000 IU/day or more over an extended period of time such as six months or longer), or over-correction of vitamin D deficiency (seen with intakes of about 77,000 IU/day for two months).
While vitamin D toxicity is possible to achieve from supplements, it is not possible when generating vitamin D from sun exposure. In fact, the pre-vitamin D made by sunlight can also be destroyed by sunlight, and converted into other molecules after a maximum amount of vitamin D3 has been created.
In other words, sunlight provides the fail-safe where the excess vitamin D3 can be broken down by UV light directly within the external layer of the skin before making it into the bloodstream.
Make Sure You Are Getting Enough of Both Sunshine & Vitamin D
It is important to incorporate safe, sensible sun exposure into a regular routine, just as it is important to make sure you are getting enough vitamin D. Because the sun produces many health-benefiting molecules in addition to vitamin D, sunshine exposure cannot be replaced with taking a supplement.
As Dr. Holick states in his videos above, it is important not to stop supplementing with vitamin D during the summer. Most people do not make enough vitamin D from sunshine alone, due to their lifestyle and other factors, and therefore must rely on supplementation to maintain optimal vitamin D levels of 40-60 ng/ml (100-150 nmol/L).